Canada’s opioid crisis has escalated to a public health emergency over the past decade, with overdose deaths reaching alarming levels. In the past eight years, over 50,000 opioid-related fatalities were reported nationwide, with British Columbia bearing the brunt of the crisis. The province’s overdose death rate remains among the highest in Canada, highlighting a challenging reality that shows no signs of abating. Within this harrowing landscape, naloxone—a life-saving medication that reverses opioid overdoses—has emerged as a pivotal tool in harm reduction strategies.
Naloxone’s role in mitigating the opioid crisis cannot be overstated. When administered promptly, it blocks the effects of opioids on the brain, effectively restoring normal breathing in individuals experiencing an overdose. Its accessibility has become a matter of life and death, particularly in regions like Vancouver’s Downtown Eastside, where overdoses occur at an alarming rate. Through take-home naloxone programs and community-based training, the medication has empowered ordinary citizens to act as first responders, significantly increasing survival rates.
This investigation analyzes naloxone’s evolving role in Canada’s response to the opioid epidemic. By exploring its history, mechanism, distribution, and challenges in ensuring equitable access, we aim to present a comprehensive understanding of its impact. In doing so, this article will shed light on the critical importance of naloxone in harm reduction while addressing broader systemic issues that continue to fuel the opioid crisis.
Understanding Naloxone and How It Works
Naloxone, often referred to as the “Lazarus drug,” is a medication designed to rapidly reverse the effects of opioid overdoses. It functions by binding to the same receptors in the brain that opioids target, effectively displacing the opioids and halting their depressive effect on the central nervous system. The primary danger in opioid overdoses stems from respiratory depression, which can lead to brain damage or death if untreated. Naloxone restores normal respiration within minutes, making it a critical life-saving intervention in overdose situations.
Historical Development: From the Lab to the Frontlines
Naloxone’s origins can be traced back to the 1960s, when Dr. Jack Fishman, a chemist at the Memorial Sloan Kettering Cancer Center in New York, developed the compound while researching opioid antagonists. Initially intended as a tool for medical professionals to reverse opioid overdoses in clinical settings, naloxone gained broader significance as opioid use—and subsequent overdose deaths—rose dramatically in the late 20th and early 21st centuries. Its adoption in harm reduction strategies marked a shift toward community-level overdose response, with take-home naloxone kits becoming increasingly available across Canada and globally.
Forms of Naloxone: Injectable vs. Nasal Spray
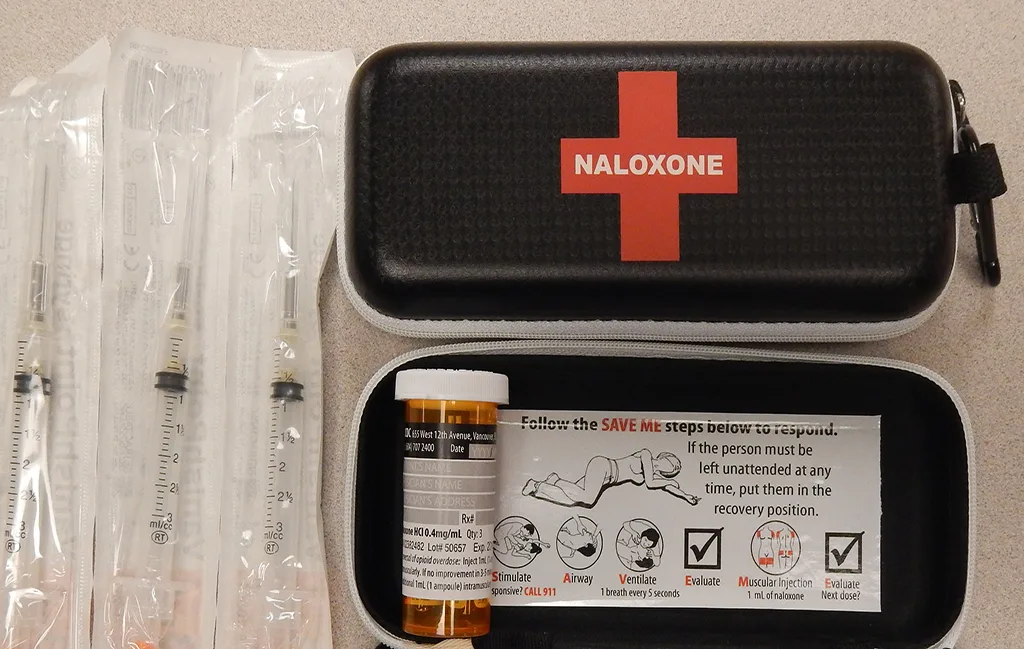
Naloxone is available in two primary forms: injectable and nasal spray.
- Injectable Naloxone:
Injectable naloxone has long been the standard method of administration. It is typically supplied in ampoules or pre-filled syringes and requires some basic training for effective use. The injectable form is cost-effective and widely distributed through take-home naloxone programs. However, its reliance on proper technique has made accessibility and usability a concern in high-stress situations.
- Nasal Spray Naloxone:
In response to usability challenges, nasal spray naloxone—marketed as Narcan—was introduced as a more user-friendly alternative. It requires no assembly or specialized training, making it ideal for laypersons responding to an overdose. Studies have shown that nasal spray naloxone is equally effective in reversing overdoses, though its higher cost has limited widespread distribution compared to injectable forms.
Both forms have been instrumental in saving lives, and their increasing availability reflects a growing recognition of naloxone’s importance in public health strategies. As Canada’s opioid crisis continues to claim lives, ensuring that naloxone remains accessible, affordable, and well-understood by the public is paramount.
The Opioid Crisis in British Columbia and the Urgent Need for Solutions
British Columbia remains at the epicentre of Canada’s opioid crisis, bearing a disproportionate burden of overdose fatalities. The province declared a public health emergency in 2016 in response to a surge in opioid-related deaths mainly driven by the proliferation of fentanyl and other synthetic opioids in the drug supply. Despite government interventions and harm reduction initiatives, the crisis continues unabated, underscoring the urgent need for expanded access to naloxone and other life-saving measures.
Sobering Statistics of Overdose Fatalities
According to the latest data from the British Columbia Coroners Service, the province recorded over 2,300 illicit drug toxicity deaths in 2023 alone. The per capita rate of overdose deaths in BC is one of the highest in Canada, with approximately 45 deaths per 100,000 people. Notably, fentanyl was detected in more than 80% of these fatalities, highlighting the lethal potency of the synthetic opioid and the challenge of combating such a rapidly evolving public health threat.
Certain regions are hit harder than others. Vancouver, notably the Downtown Eastside, has become a focal point of the crisis. The DTES is home to a high concentration of marginalized populations, including individuals experiencing homelessness and those struggling with addiction. The area’s unique socio-economic challenges have made it especially vulnerable to the devastating effects of opioid overdoses. In this context, naloxone has emerged as a critical tool in harm reduction, with community-led initiatives distributing thousands of kits annually to residents and outreach workers.
Naloxone’s Role in Reducing Overdose Deaths
Naloxone has played an instrumental role in reducing the immediate harm caused by opioid overdoses in BC through the province’s Take Home Naloxone (THN) Program, more than 1.5 million doses of naloxone have been distributed since its inception. This widespread availability has saved countless lives, with data showing that naloxone administration by laypersons prevented tens of thousands of potential fatalities.
However, while naloxone can reverse overdoses in the moment, it is not a cure for addiction. Experts stress that without addressing the underlying factors driving the crisis—poverty, mental health issues, and an unregulated toxic drug supply—naloxone alone cannot stem the tide of overdose deaths. Nevertheless, its role in keeping people alive long enough to seek treatment remains indisputable.
Community Engagement and Grassroots Solutions
In areas like the DTES, naloxone distribution efforts rely heavily on grassroots organizations, peer-support networks, and harm reduction advocates. These groups are on the front lines, ensuring that naloxone kits are readily available to those at the highest risk. Additionally, regular training sessions teach residents how to administer naloxone correctly, empowering the community to act swiftly in overdose situations.
As the crisis persists, British Columbia’s experience with naloxone offers valuable lessons for other regions facing similar issues. The province’s efforts demonstrate that while naloxone is not a silver bullet, it is a vital component of a broader harm reduction strategy to minimize loss of life.
Take-Home Naloxone Programs in Canada
Take-home naloxone programs have become a cornerstone of Canada’s harm reduction strategy in response to the opioid crisis. Initially launched as a regional effort, these programs have expanded nationwide, ensuring that naloxone is readily accessible to individuals at risk of witnessing or experiencing opioid overdoses. The goal is simple yet critical: provide life-saving tools to the public to reduce overdose fatalities in both urban and rural settings.
The Rise of Take-Home Naloxone Programs
The concept of take-home naloxone first gained traction in Canada in 2005 with a pilot program in Alberta aimed at equipping opioid users and their families with naloxone kits. By 2012, British Columbia followed suit with its own THN initiative, driven by alarming increases in opioid-related deaths. The BC program, managed by the British Columbia Centre for Disease Control (BCCDC), became a model for other provinces due to its comprehensive distribution network and emphasis on community engagement.
By 2016, amid a worsening opioid crisis, the federal government declared a public health emergency and actively promoted the expansion of THN programs across the country. Today, every province and territory in Canada offers some form of take-home naloxone program, supported by local health authorities and non-profit organizations. These programs have distributed millions of naloxone kits and trained thousands of Canadians in overdose response techniques.
Key Players in Distribution Efforts
Take-home naloxone programs rely on a wide network of organizations to distribute kits and provide training. In British Columbia, public health authorities play a leading role, working in partnership with pharmacies, community health centers, and harm reduction groups. Non-profit organizations such as the Canadian Drug Policy Coalition and local advocacy groups are instrumental in reaching marginalized communities, especially in areas with high overdose rates, like Vancouver’s Downtown Eastside.
Pharmacies have also become critical distribution points. Since 2016, naloxone kits have been available for free at pharmacies across Canada without a prescription. This accessibility has significantly increased public awareness and usage of naloxone, empowering individuals from all walks of life to act as first responders during an overdose. However, distribution alone is not enough—training remains a vital component of these programs. Many organizations host workshops and outreach sessions to ensure that recipients of naloxone kits are confident in their ability to use them correctly during a crisis.
Successes and Ongoing Challenges
The success of take-home naloxone programs is evident in the number of lives saved. In British Columbia alone, data from the BCCDC indicates that between 2012 and 2023, naloxone kits were used to reverse over 65,000 overdoses. Nationally, health experts credit these programs with preventing tens of thousands of deaths and helping to normalize harm reduction as a public health priority.
Despite these successes, significant challenges remain. One major issue is the stigma surrounding drug use, which can deter individuals from seeking naloxone kits or administering them in public settings. Rural and remote communities also face barriers in accessing naloxone due to limited healthcare infrastructure. Critics argue that while THN programs save lives, they are a reactive solution that fails to address the root causes of the crisis, such as the toxic drug supply and lack of comprehensive addiction treatment services.
Moreover, maintaining consistent funding for these programs is a persistent concern. While initial federal and provincial investments were robust, some advocates worry about long-term sustainability, particularly as demand for naloxone continues to grow amid ongoing waves of opioid-related deaths.
Expanding Naloxone Access through Training and Community Outreach
Ensuring widespread access to naloxone is only part of the equation. Equally critical is equipping individuals with the knowledge and confidence to administer it effectively during an overdose. Across Canada, various training programs have emerged to bridge this gap, offering practical education on naloxone use and overdose prevention. However, challenges such as stigma, fear, and logistical barriers remain obstacles in reaching the most vulnerable populations.
Naloxone Training Programs Equipping Communities with Critical Skills
Training programs like “Naloxone 101” play a pivotal role in fostering a culture of preparedness. These programs, offered by public health authorities, harm reduction organizations, and non-profits, provide participants with essential skills such as identifying an overdose, administering naloxone, and performing rescue breathing. The Naloxone 101 Training Course, for example, breaks down complex medical procedures into simple, actionable steps, ensuring that even those with no medical background can confidently intervene during an emergency.
Training sessions are often conducted in person at community health centers and pharmacies or through online platforms for greater reach. Many sessions are complemented by the free distribution of naloxone kits, ensuring that participants leave with the knowledge and the tools to act. The emphasis on hands-on practice, scenario-based learning, and clear, jargon-free language makes these programs highly effective in building public confidence. In British Columbia, the popularity of such initiatives has contributed significantly to the high rate of bystander intervention during opioid overdoses.
Overcoming Barriers to Reach Marginalized Communities with Naloxone
Marginalized communities, particularly those experiencing homelessness or living in poverty, are disproportionately affected by the opioid crisis. Ensuring that naloxone reaches these populations requires targeted outreach and partnerships with frontline organizations. In Vancouver’s Downtown Eastside, where overdose rates are among the highest in Canada, community health workers and peer-led initiatives are vital to expanding access.
Mobile health units, pop-up clinics, and peer networks have proven effective in delivering naloxone and training directly to at-risk individuals. These efforts address logistical barriers such as lack of transportation and fear of accessing formal healthcare settings. Peer trainers—often individuals with lived experience—play a unique role in building trust within marginalized communities, helping to normalize naloxone use and reduce the stigma around drug-related interventions.
Despite these successes, barriers remain. Language, cultural differences, and mistrust of authority can hinder community engagement. To counter this, public health agencies have begun collaborating with cultural groups and Indigenous organizations to deliver culturally sensitive training programs tailored to specific needs. These initiatives aim to create a more inclusive approach that recognizes the diverse realities faced by different populations.
Shifting Public Perception by Confronting Stigma and Fear Around Naloxone
The stigma around drug use remains a significant hurdle in the effective deployment of naloxone. Many individuals hesitate to carry or use naloxone due to fear of being judged or penalized. This stigma is compounded by misconceptions about naloxone encouraging drug use despite clear evidence showing that its primary function is to save lives, not enable behaviour.
Public awareness campaigns have been instrumental in shifting perceptions. Messaging that frames naloxone use as an act of compassion and responsibility has gained traction, particularly in urban centers heavily impacted by the opioid crisis. Furthermore, legal protections such as Good Samaritan laws, which protect bystanders from prosecution when administering naloxone during an overdose, have alleviated some fears. However, more work is needed to ensure that people feel empowered rather than criminalized when offering aid.
Tackling stigma requires a multi-faceted approach, including education, public messaging, and community support. By normalizing naloxone use and fostering empathy, society can create an environment where saving a life is not met with hesitation but with urgency and confidence.
The Role of Community in Saving Lives
While government policies and healthcare systems are vital in addressing the opioid crisis, it is often ordinary citizens who find themselves on the frontlines of saving lives. Community members trained in naloxone administration have become everyday heroes, stepping in during critical moments to prevent fatal overdoses. These grassroots efforts, driven by compassion and necessity, underscore the irreplaceable role of communities in harm reduction.
Everyday Heroes Saving Lives with Naloxone
Across British Columbia, stories abound of everyday people using naloxone to save lives. From bystanders in public parks to neighbours stepping in during emergencies, their quick actions have prevented countless tragedies. In one notable case, a Vancouver resident named Jason—trained through a local naloxone program—recounted how he saved a friend’s life by administering naloxone during a sudden overdose. “I didn’t think, I just acted. The training kicked in,” Jason shared in a public testimony.
These stories illustrate the power of community-led harm reduction. By equipping ordinary people with naloxone kits and the knowledge to use them, communities are reducing fatalities and fostering a culture of care and intervention. According to provincial health data, areas with high community engagement in naloxone programs report significantly lower overdose mortality rates., where the impact of crime is deeply felt in places like the Downtown Eastside, the stakes are high. Ensuring that effective and equitable reforms will be crucial for building safer, more resilient communities. As the debate continues, one thing is clear: the status quo is no longer an option.
Community-Led Harm Reduction Expanding Beyond Distribution
In response to the escalating opioid crisis, many community-driven initiatives have stepped beyond mere naloxone distribution to offer holistic support. Organizations like VANDU (Vancouver Area Network of Drug Users) and Portland Hotel Society run peer-led harm reduction programs that combine naloxone training with education on safer drug use, overdose prevention, and access to health services.
These initiatives often operate in areas with high rates of opioid use, such as Vancouver’s Downtown Eastside, where traditional healthcare systems may not always be accessible or trusted by residents. Peer-led efforts have proven particularly effective in bridging this gap. Employing individuals with lived experience creates a safe, non-judgmental space for those in need, fostering trust and engagement.
Moreover, mobile outreach teams—many operated by non-profits—patrol high-risk areas to offer on-the-spot naloxone administration, distribute clean supplies, and connect individuals to support services. This proactive approach reduces the burden on emergency services and ensures that help is available where needed most.
Peer-Led Programs Building Trust in Harm Reduction Efforts
At the heart of successful community initiatives are peer-led programs—efforts driven by people who have firsthand experience with drug use and the associated challenges. Peer workers serve as educators, responders, and role models, demonstrating that recovery is possible. Their involvement is critical in reducing stigma and building trust, especially in marginalized communities that may view traditional authorities with skepticism.
Peer-led naloxone programs have been credited with boosting the effectiveness of harm reduction strategies across British Columbia. By delivering training in a culturally sensitive manner and addressing the unique needs of various groups, peer workers have ensured that naloxone reaches those who need it most. These programs also play a pivotal role in post-overdose care, offering emotional support and guidance on accessing treatment or rehabilitation services.
The role of the community in combating the opioid crisis cannot be overstated. While systemic reforms and increased funding remain essential, grassroots efforts remain lifelines for many. Empowering communities with tools, knowledge, and empathy ensures that more lives are saved, one intervention at a time.
Limitations and Challenges Beyond the Miracle Drug
While naloxone has earned its reputation as a lifesaving intervention in the opioid crisis, it is not a panacea. Limitations in its efficacy, distribution challenges, and the emergence of more complex drug combinations have exposed critical gaps in current harm reduction strategies. This section delves into the circumstances where naloxone might fall short, the barriers to its widespread use, and innovative advancements to enhance overdose prevention.
Limitations of Naloxone with the Rise of Benzo-Dope and Xylazine
Naloxone’s mechanism of action—blocking opioid receptors to reverse respiratory depression—makes it highly effective against pure opioid overdoses. However, its efficacy diminishes significantly when dealing with polysubstance overdoses involving drugs like benzo-dope (a combination of benzodiazepines and opioids) and xylazine (an animal tranquillizer increasingly found in illicit drug supplies). These substances do not respond to naloxone because they affect different receptors in the central nervous system.
According to data from the British Columbia Centre on Substance Use, over 40% of recent overdose deaths in the province involved benzo-dope or xylazine. Unlike opioid overdoses, where naloxone can quickly restore breathing, these mixed-drug overdoses require additional interventions, such as mechanical ventilation and benzodiazepine antagonists. This complicates the role of naloxone, highlighting the need for more comprehensive overdose response strategies.
Additionally, repeated doses of naloxone are sometimes required when potent synthetic opioids like fentanyl or carfentanil are involved. Even multiple administrations may not suffice in extreme cases, leading to fatal outcomes despite timely intervention. These realities underscore the urgency of expanding the toolkit for overdose response beyond naloxone alone.
Barriers to Distribution, Awareness, and Usage
Despite widespread acknowledgment of naloxone’s life-saving potential, issues with distribution and awareness persist. According to a national report on take-home naloxone programs, certain rural and remote communities in Canada face limited access to naloxone kits. Geographic isolation, combined with a lack of trained personnel, hampers timely intervention during overdoses in these areas.
Additionally, stigma remains a significant barrier. Fear of judgment, legal repercussions, or involvement with law enforcement often deters people from seeking naloxone or intervening during an overdose. Even in urban centers with high naloxone availability, hesitancy to act can result in preventable deaths. A study conducted in Vancouver’s Downtown Eastside found that nearly 25% of bystanders who witnessed an overdose failed to administer naloxone due to uncertainty or fear of doing something wrong.
Efforts to address these challenges have included public education campaigns and the integration of naloxone training into community programs. However, gaps remain in ensuring that everyone—from casual bystanders to first responders—feels confident and empowered to use naloxone when needed. Increasing trust and reducing stigma through peer-led outreach and culturally sensitive training programs could enhance naloxone’s impact in high-risk communities.
Innovations in Overdose Prevention Technology
Recognizing the limitations of traditional naloxone delivery methods, researchers and pharmaceutical companies are exploring new technologies to improve overdose prevention. Among the most promising advancements are naloxone implants and naloxone patches.
Naloxone implants, which release a steady dose of the drug over an extended period, are designed to offer continuous protection for individuals at high risk of overdose. These implants could be particularly beneficial for people in treatment programs or those recently released from incarceration—groups that face heightened overdose risks due to reduced opioid tolerance.
Similarly, naloxone patches function like transdermal drug patches, delivering a controlled dose of naloxone through the skin. While still in experimental stages, these patches aim to provide a proactive defence against accidental overdoses by maintaining a baseline level of naloxone in the bloodstream.
Another innovative approach involves wearable overdose detection devices with sensors monitoring respiratory patterns. When a potential overdose is detected, these devices can automatically administer naloxone or alert emergency responders. Pilot programs testing such technology in Vancouver and Toronto have shown promising results, with early interventions preventing severe outcomes in several cases.
While these advancements offer hope, they also raise questions about accessibility and cost. Ensuring equitable distribution of new technologies will be essential to their success in addressing the opioid crisis. Without proper funding and support, these innovations risk becoming privileges for the few rather than widespread solutions for all.
Naloxone Policies and Health Authority Initiatives in Canada
Efforts to address the opioid crisis in Canada have largely focused on expanding harm reduction strategies, with naloxone distribution playing a pivotal role. Federal and provincial governments and regional health authorities have launched numerous initiatives to improve access to naloxone. However, challenges remain in ensuring consistent policy implementation, equitable distribution, and sustained funding. This section examines key policies and ongoing efforts and calls for a more comprehensive harm reduction framework.
Canada’s Federal Policies on Naloxone and Harm Reduction
At the federal level, Health Canada has prioritized naloxone distribution as part of its broader opioid response strategy. In 2016, naloxone was added to the Prescription Drug List (PDL), making it available without a prescription across the country. This move aimed to remove barriers for individuals at risk of overdose and increase naloxone’s presence in community settings. Additionally, Health Canada introduced measures to facilitate the importation of nasal spray formulations, such as Narcan, to complement existing injectable kits.
Federal funding has also supported the establishment of supervised consumption sites, which often distribute naloxone kits and provide overdose response training. As of 2024, over 40 federally approved supervised consumption sites operate across Canada, many concentrated in high-risk regions like British Columbia. These sites serve as crucial distribution points for naloxone while offering a safe environment for individuals using substances.
Despite these efforts, advocates have called for further policy improvements. Key demands include increased federal funding for community-based naloxone programs, greater support for peer-led initiatives, and improved data collection on naloxone distribution and usage. Critics argue that while current policies focus on immediate harm reduction, they fall short in addressing the systemic causes of the opioid crisis, such as poverty, inadequate mental health care, and housing insecurity.
Naloxone Distribution Initiatives in British Columbia
British Columbia has been forefront of harm reduction efforts, particularly in naloxone distribution. The province launched its Take Home Naloxone Program in 2012, becoming one of the first jurisdictions in North America to implement such an initiative. Since its inception, the program has distributed over 1.5 million naloxone kits and trained thousands of individuals in overdose response. The THN program is coordinated by the BC Centre for Disease Control and operates through a network of pharmacies, community organizations, and healthcare providers.
In addition to the THN program, BC’s government has invested in expanding overdose prevention services, including mobile units and pop-up clinics that distribute naloxone kits in underserved areas. A 2023 report by the Ministry of Mental Health and Addictions highlighted that over 80% of opioid-related deaths in the province occurred indoors, often in private residences. This statistic underscores the importance of making naloxone readily available in public settings and homes.
However, concerns remain regarding the sustainability of these programs. While the province has allocated significant resources to harm reduction, some stakeholders have criticized the lack of long-term funding guarantees. Others point out that rural and remote communities continue to face tremendous barriers to accessing naloxone, with distribution networks heavily concentrated in urban centers like Vancouver and Victoria.
Regulatory Bodies and the Push for Expanded Harm Reduction
Regulatory bodies, such as the College of Pharmacists of British Columbia, are critical in ensuring naloxone’s accessibility. Since the deregulation of naloxone, pharmacies have become key distribution points, with many offering free naloxone kits and training to customers. Additionally, the college has worked with health authorities to develop guidelines for pharmacists on identifying at-risk individuals and providing targeted support.
Calls for expanding harm reduction efforts beyond naloxone are gaining momentum. Advocates argue that while naloxone is an essential tool, it addresses only the immediate symptoms of the opioid crisis. Proposals include scaling up safer supply programs, increasing funding for mental health services, and implementing drug decriminalization policies. In early 2024, BC piloted a safer supply initiative in collaboration with health authorities, providing prescribed alternatives to toxic street drugs. Early evaluations suggest that such programs can reduce overdose rates and improve the overall well-being of participants.
Regulatory bodies are also exploring innovative models for naloxone distribution, such as integrating overdose prevention services into primary care clinics and expanding workplace naloxone programs. By embedding harm reduction into everyday healthcare and employment environments, policymakers hope to create a more proactive and inclusive approach to combating the opioid crisis.
Global Approaches to Naloxone and What Canada Can Learn
The opioid crisis is not unique to Canada. Across the globe, countries have grappled with surges in opioid-related deaths, leading to varying harm reduction strategies. Examining international approaches provides valuable insights into how Canada can strengthen its naloxone programs and broader harm reduction efforts.
Italy’s Pioneering Approach to Naloxone Distribution
Italy is an early leader in adopting naloxone as a harm reduction tool. In the 1980s, amidst a growing heroin crisis, the Italian government introduced naloxone as a publicly accessible medication. Unlike many countries where naloxone distribution was initially restricted to healthcare professionals, Italy implemented a community-centred approach, ensuring naloxone kits were available to at-risk populations through local harm reduction centers. By the late 1990s, naloxone could be purchased over the counter in Italian pharmacies, a policy that remains in effect today.
The Italian model is noteworthy for its sustained emphasis on low-barrier access and public education. Campaigns focused on destigmatizing naloxone use have resulted in widespread public acceptance. A 2020 study published in the European Journal of Public Health noted that Italy’s naloxone programs contributed significantly to reducing opioid overdose mortality, with cities like Milan and Rome reporting consistent declines in opioid-related deaths over a decade. The Italian experience underscores the importance of early adoption, public education, and ensuring that naloxone is as widely accessible as possible.
Harm Reduction Success in the UK and Australia
The United Kingdom and Australia have also implemented robust harm reduction strategies, with naloxone playing a central role. In the UK, the Take Home Naloxone Program was launched in 2011 and has since expanded across all four nations: England, Scotland, Wales, and Northern Ireland. Scotland, in particular, has been at the forefront, given its disproportionately high rate of opioid-related deaths compared to other parts of the UK. A 2023 report by Public Health Scotland revealed that over 45,000 naloxone kits were distributed in the previous year alone, saving hundreds of lives.
Australia adopted a similar approach with its Naloxone Pilot Program, which was launched in 2019. Initially covering a handful of states, the program was expanded nationwide in 2022 due to its success. The Australian model focuses heavily on integrating naloxone distribution into existing healthcare services, such as general practitioner clinics and emergency departments, ensuring that individuals who have experienced non-fatal overdoses are equipped with naloxone upon discharge. Furthermore, Australia has invested significantly in peer-led outreach programs, recognizing that community trust is crucial for effective harm reduction.
Both countries highlight the critical role of comprehensive policy frameworks that go beyond distribution to include training, public awareness, and ongoing support for users. Additionally, the integration of naloxone into broader healthcare services, as seen in Australia, serves as a potential model for Canada to emulate, particularly in provinces like British Columbia, where healthcare systems are already stretched thin.
Key Takeaways for Canada
While Canada has made significant strides in naloxone distribution, international comparisons reveal areas for improvement. Italy’s early adoption and low-barrier access model demonstrate the long-term benefits of making naloxone readily available without prescription, paired with sustained public education efforts. Similarly, the UK and Australia showcase the effectiveness of embedding naloxone programs within broader healthcare systems and leveraging community partnerships for outreach and education.
Canada can learn from these models by focusing on three key areas:
- Removing Barriers to Access: Although naloxone is widely available across Canada, certain regions still face logistical and systemic hurdles. Drawing inspiration from Italy, policymakers could explore expanding over-the-counter naloxone availability in rural and remote communities.
- Enhancing Integration into Healthcare Services: The Australian model of integrating naloxone distribution into hospital discharge protocols and primary care settings could be particularly effective in high-risk areas like Vancouver’s Downtown Eastside.
- Expanding Public Awareness Campaigns: Stigma remains a significant barrier to naloxone use in Canada. Broad, sustained public education campaigns, similar to those in Italy and Scotland, could help normalize naloxone use and empower more citizens to carry and administer it during emergencies.
As Canada continues to battle its opioid crisis, learning from international success stories can help refine its harm reduction strategies. While naloxone is not a silver bullet, its role as a life-saving intervention cannot be overstated. By adopting best practices from around the world, Canada can improve its efforts to curb overdose deaths and build a more robust harm reduction framework.
Building a Future Where Naloxone Saves More Lives
Naloxone has emerged as an indispensable tool in Canada’s ongoing struggle against opioid overdoses. However, while its role in saving lives is beyond dispute, the scope of its impact depends largely on how effectively it is implemented within a broader harm reduction framework. As this investigation has shown, naloxone alone cannot reverse the crisis—it must be part of a more extensive, systemic approach that addresses both immediate overdose risks and the root causes of addiction.
Next Steps for Increasing Naloxone Availability Across Canada
The expansion of naloxone programs has been significant, but gaps remain in rural and underserved communities. While urban centers like Vancouver have robust distribution networks, accessibility in remote areas remains challenging. Ensuring that naloxone reaches every corner of the country requires sustained funding, logistical improvements, and increased collaboration between government bodies, healthcare providers, and community organizations.
Equally important is the continued emphasis on education and training. Programs like Naloxone 101 are critical in equipping individuals with the knowledge to act swiftly in emergencies. Expanding these initiatives to reach a wider audience, including workplaces, schools, and public spaces, will be key in normalizing naloxone use and empowering bystanders to save lives. Success lies in distributing the medication and building confidence among potential users.
Integrating Harm Reduction with Long-Term Solutions
While naloxone addresses the immediate threat of overdose, sustainable progress hinges on integrating harm reduction efforts with long-term solutions. Investments in affordable housing, mental health services, and addiction treatment are essential for breaking the cycle of substance dependence. Without addressing these underlying factors, the reliance on naloxone as an emergency measure risks becoming a stopgap rather than a stepping stone toward lasting change.
Furthermore, as opioid formulations evolve—introducing new challenges like benzo-dope and xylazine overdoses—the harm reduction landscape must adapt accordingly. Continued research into innovative solutions, such as long-acting naloxone formulations and overdose detection technologies, will ensure that Canada remains prepared for emerging threats. Policymakers must prioritize the distribution of existing resources and the development of next-generation interventions.
A Lifesaving Strategy in the Fight Against Overdoses
Naloxone represents hope amid a public health crisis. Its success in reducing overdose deaths is undeniable, yet its potential remains tied to broader systemic efforts. Building a future where naloxone saves more lives requires ongoing vigilance, innovation, and a commitment to immediate harm reduction and long-term care.
This guide aimed to provide a comprehensive understanding of naloxone, from its pharmacological roots to its role in Canada’s harm reduction strategy. As the opioid crisis continues to evolve, naloxone stands as a critical line of defence, but it cannot stand alone. By enhancing accessibility, expanding education, and addressing systemic inequities, Canada can strengthen its lifesaving framework and offer tangible hope to those most at risk.
Kris has been at the forefront of Downtown Eastside initiatives for over 15 years, working to improve the neighbourhood. As a consultant to several organizations, he played a key role in shaping harm reduction strategies and drug policies. A strong proponent of decisive action, Kris’s work focuses on driving tangible change and advocating for solutions that address the complex challenges facing the community.






Leave a Comment